“Fentanyl has killed more Americans than the wars in Vietnam, Iraq, and Afghanistan combined,” reported The New York Times in an October 2023 article.
According to the same Times article, “Some Key Facts About Fentanyl,” fentanyl is 50 times more powerful than pure heroin and “107,888 people died from drug overdoses in the U.S. in 2022 and 73,798 involved fentanyl or a similar drug.”
Brenda Conlan, who you may know as The Drug Lady, is a drug and alcohol educator. She warns “fentanyl is killing around 200 Americans every single day. It’s like a major plane crash every day.”
Our students are being educated by the school, in health class, about fentanyl, and some are also being educated by their parents (but not all). Unfortunately, some of our faculty and staff have known loved ones who have passed away or been harmed by fentanyl, and some have even been exposed to fentanyl themselves.
To get more information about our school community and the fentanyl crisis, we sent out a Google form, and received 57 responses. One response said “A girl in my class at [a previous] school last year overdosed on fentanyl in the gym and it was really scary and the whole school was put on lockdown. Luckily she survived, but it brought attention to the dangers of fentanyl and now all the teachers have narcan in their classrooms.”
Another response said that “My best friend’s daughter (who was in her mid 20’s) died of an accidental overdose in 2021. She had struggled with addiction since high school. It has been devastating for everyone close to her.”
Seven percent of people said yes when asked if they have been exposed to fentanyl themselves, and 67.9% said yes when asked if their parents have talked to them about the topic of fentanyl. Also, 67.9% said yes when asked if they think the school does a good job educating on the topic of fentanyl.
When we asked teachers if there was anything else they would like to share, and one said “As a teacher, I am not sure if the school does a good job educating about fentanyl. They don’t educate the teachers, as far as I know, but perhaps they educate the students.” Another person said that “I believe [students in this current generation] are in a uniquely and particularly dangerous position compared to generations before you–particularly with respect to addiction-inducing exposures and access.”
How is our school administration managing and dealing with the crisis? To get some insight, we interviewed Dr. Stanton who is the director of health services here at SSSAS. One of our biggest questions for her was about Narcan and whether or not the school carries it at the campuses. In response to this, Dr. Stanton informed us that “we have had Narcan on our campuses for the last six years. We added to our medical supply due to the increase of narcotic overdoses (accidental and intentional) that have been occurring across the nation. We felt that we needed to be in a position to administer Narcan if something were to happen on our campuses. All three divisions have Narcan available if it may be needed.” When asked about whether or not our school has ever needed to administer the Narcan, Dr. Stanton’s response was, luckily, no.
The drug lady, Brenda Conlan said that Naloxone is a medicine that will reverse any opioid overdose, and is most commonly found in the nasal spray Narcan. This medication saves lives, and has no down side; “That’s the beauty of Narcan. It really only does one thing, it reverses the effects of opiates only” said Conlan.
We wanted to know about how our school community is involved with giving out information about fentanyl and how it is tough so we interviewed Mrs. Mazur to gain a further understanding. Mrs.Mazur is a health teacher here at SSSAS, and she teaches 10th and 12th grade health classes. Even though she teaches both of these grades the way they go about learning about drugs and specifically fentanyl is different. The 10th graders have a two-day lesson with Brenda Conlan to discuss topics like fentanyl and drug usage in general. However, the 12th graders learn in class what fentanyl is, the risks of it, signs of an overdose, and how you would go about helping somebody.
She also has children in college so we asked Mrs. Mazur about how she goes about teaching her own children about fentanyl. She emphasizes how risky drugs are, especially with fentanyl, and with drugs being found in many places and often being mixed with other drugs or cross contamination between drugs. She also mentioned how to get help and how to help other people to prevent overdose. Mrs. Mazur mentions how helping someone depends on the situation. For example, whether they are just using drugs or if they are helping somebody else who has had an overdose. She explains how some use drugs simply because they are curious, and other times people will use drugs as a self coping mechanism.
Mrs. Mazur states that for people who are just curious it’s more important to let them understand the risk, and if it is a self coping mechanism that it is important to get them help with whatever they’re coping with. She says that “Treating drug use can be a bit tricky but we want to make sure that students understand the risk, the support, and different avenues of health.”
We concluded the interview with more about her personal experience when it comes to fentanyl and people she knows who have encountered it. She mentions that one of her students has had family members that are impacted by fentanyl. Mrs. Mazur also brought up that her brother-in-law is a drug addict and how he encountered fentanyl with the drugs he uses. She mentions how this is tough on her family. “We have a fear in our family that one day we’ll get the phone call that my brother-in-law passed.” She continued, “Once somebody starts using at that level you’re not really dealing with the person anymore you’re dealing with the drugs and that’s a whole different ball game.”
Additionally, we wanted to get someone in the medical field to share their professional opinions and give us insight on the seriousness of the issue. We interviewed Hartley Wenger, a Saints parent, who is an acute and critical care Clinical Nurse Specialist at INOVA Fairfax, in the 4th busiest emergency department in the entire country. She specializes in pediatric critical care medicine, and also helps manage all the critical patients who present to the ED. She says that as an ER nurse she has lots of exposure to patients with drug addiction and/or overdose. She says that on the national level “the most up-to-date data from 2021 indicates that there were more than 106,000 opioid related deaths in the United States that year.” She says that in her department, they have seen almost 150 overdose cases in the last year.
When asked about the signs of fentanyl overdose, she said “Signs of fentanyl overdose include pale, clammy skin, blue or gray colored lips or fingernails, inability to wake someone up even when you shake the person, and slow breathing or no breathing at all. If you see these signs, it may be an opioid overdose and you should immediately call 911 and stay with the person until help arrives.”
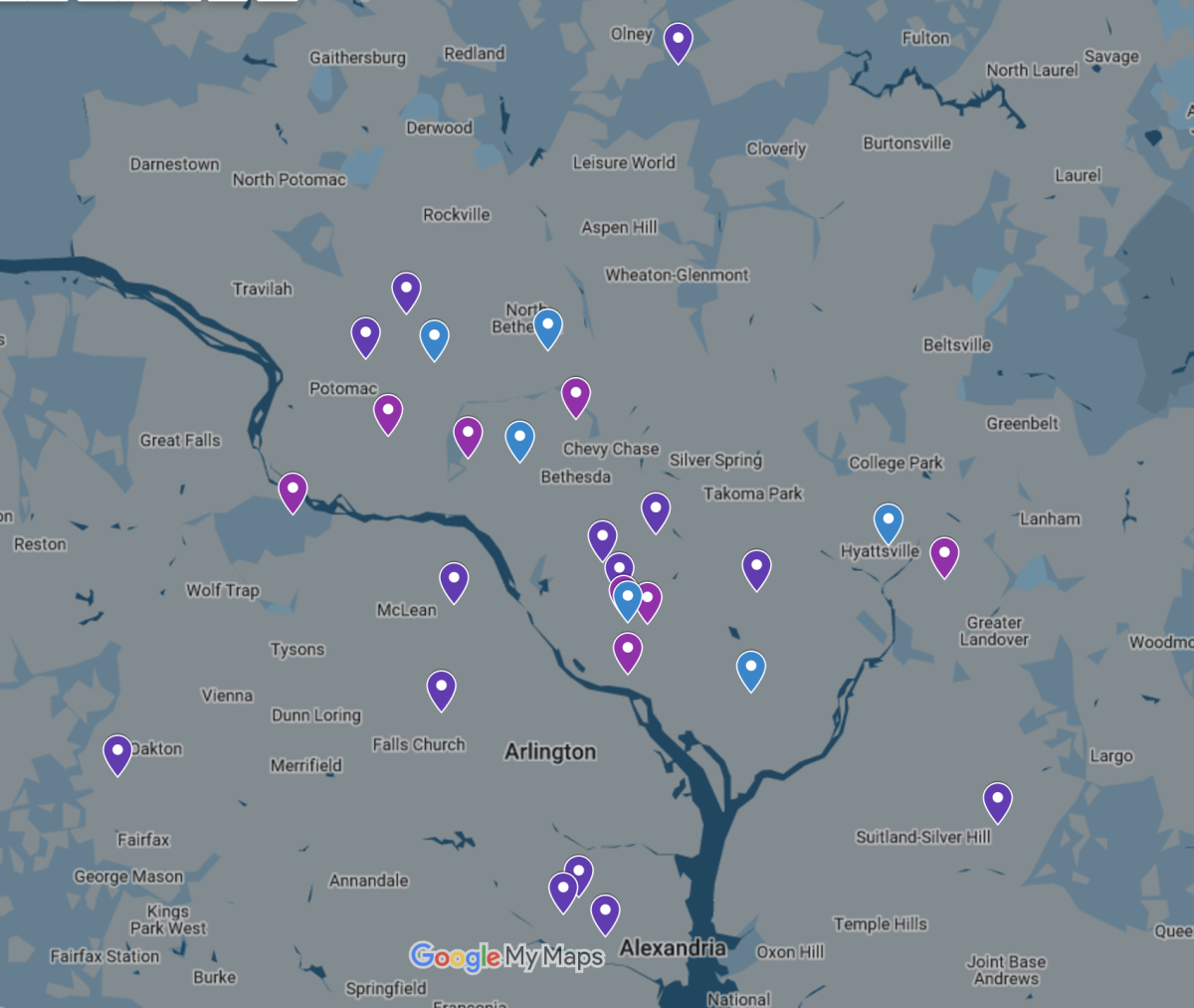
We also spoke to two students who attend West Potomac High School, and asked them about their experiences with fentanyl. They were all in agreement that the issue is quite severe and prevalent in their school community. They recalled an accidental fentanyl overdose that occurred two years ago in the parking lot of their school. A student at their school accidentally overdosed on fentanyl and sadly passed away. This tragic event really made the opioid issue evident to the school community.
These students said they have never encountered fentanyl personally but say “There are a lot of kids our age who have at least tried fentanyl in small doses or other opioids without overdosing.” They feel that buying drugs that aren’t verified as real from suspicious dealers is too big a risk to take.
They also mentioned new extra security their school has introduced saying “Our school recently implemented security [guards] into the bathrooms to oversee that no one is doing any drugs.” They also mentioned how their school spoke briefly with them about what narcan (Naloxone) is, saying “Our school gave every kid an introduction to what Narcan is; after 2 years of this ongoing issue, I bet you every public school has that conversation with their students.” They said they feel that their school has to push the severity of the issue more and that it doesn’t really stick with students. “Our school tries to stop kids at our school from doing drugs during health and advisory, but the message doesn’t really reach the students.”
Brenda Conlan (the drug lady) explained that fentanyl made its way into the illegal drug supply as a cheap alternative to more expensive drugs: “A real Oxycontin, you can get $80 for that on the street. You can make a fake oxycontin for 10 cents and sell it for $80.” Conlan expressed that students are often confused with “the whole premise of why would these drug dealers kill their customers.” In reality, the drug dealers are not trying to kill their customers but as they are not pharmacists, they may struggle with dosage of fentanyl. “You might have one pill that has 10 milligrams of fentanyl… you might have another pill that only has half a milligram of fentanyl in it” It only takes 2 milligrams of fentanyl to cause an overdose.
Fentynal overdose at the teenage level is almost always accidental. Conlan really emphasized concern in online drug deals, specifically on Snapchat. Anyone selling drugs on Snapchat is not reliable, and the drug being bought has a high chance of containing fentanyl. There is also worry with how to get the drugs into the hands of the buyers. Conlan said, “doubly dangerous, because first of all, you’re buying drugs on Snapchat. But second of all, how do you get the drugs? You’re gonna have to either meet this person, or give them your address or whatever.” This type of drug deal has become so common that buyers use emojis to signify the type of drug they want and how much of it.
In Hartley Wenger’s interview she stresses the crisis by reminding us that “it only takes one time to accidentally overdose.” Lastly, she gave some very insightful information about exactly what to do if you ever see someone experiencing an overdose. She said, “ Do not hit or smack the person in an attempt to wake them up and do not place them in a bath or shower to wake them up. Don’t let the person sleep it off or leave the person alone. Instead, call 911 immediately and place the person on his or her side. Stay with the person until help arrives. If you or anyone you know is struggling with substance abuse, call the national hotline at 800-662-4357. It’s free, and confidential, and open 365 days a year.”
They say over 100,000 people a year die from preventable drug overdoses in the United States, that nearly 1 in 10 families in The United States have lost a family member to a drug overdose. For many of us, including myself, these have often seemed like distant facts with little tangible impacts on our lives. You never think you will become a part of that statistic. A fraction of a pill can cost a life.
I’ll never forget that afternoon. We had all of our bags packed, ready to return to my mother’s hometown for the long Easter weekend. I sat in the living room, waiting for my parents to come down when an eerie feeling arose. My dad is what most would consider an “airport dad”—the kind that wants to be there at least two hours early before a flight. We were nearing an hour and a half to departure, and a gut-retching feeling overcame me. From the bottom of the stairs, I heard what sounded like weeping. Immediately, my heart sank. I knew bad news was to come. As my father helped my mother down the stairs, I saw her fall to the ground, tears streaming down her face as she screamed, “Why, God, why?” I had heard this cry only a few times before; I knew its meaning. It was a cry of mourning.
As I begged my mother to tell me what was happening, tears streaming down my face, she could only yell, “Never do this to me, never, never, never….” We sat on the ground together, trying to regain composure and understand what had happened. At that moment, she said, “he’s gone.” I prodded once more, asking, “Who’s gone?”. She went on to tell me that my Aunt had just called her and that my cousin had passed away, and they didn’t know why yet. She recounted the harrowing moment his roommates had found him, prompting an urgent call to my uncle in a state of pure despair. They were unable to resuscitate him. He was gone.
As we continued our journey home to be with our family, I remember looking out at the clouds from the plane window, trying to make sense of what had happened. My cousin was not what most would label a “drug addict.” He was a young college student with a bright future ahead of him. He was the kind of person who lit up any room and who everyone knew by name. Still, like many young adults, he struggled with anxiety and depression, unsure of how to treat it. Consequently, he turned to using Xanax as a coping mechanism, not thinking it would eventually end his life.
While this habit progressed, he recognized he needed to find better ways to cope with his mental health struggles, eventually participating in rehabilitation programs, therapy, and other mental health retreats. It looked promising, and he was doing exceptionally well. Still, a poor decision one night to share a pill with his friends ended up costing him his life. Four of them split that pill. Four ways, and he was the only one that passed away. Fentanyl is everywhere and more lethal than we could ever imagine. In fact, a two-milligram dose is considered a lethal dose, similar to five to seven grains of salt. One side of a pill could test negative for fentanyl, while a tiny sliver on the other side might contain it. Fentanyl does not alter the taste, smell, or appearance of pills. It is nearly impossible to detect.
So, I ask you not to let his death be in vain. Do not take medications from anywhere other than directly from a pharmacy or sealed in a package from a retail store. It takes less than one pill, and it can take your life.